Did you know that prescription errors harm countless patients worldwide?
For instance, in the United States, which has one of the best healthcare systems, over 7,000 deaths annually occur due to prescription errors.

These numbers are likely an underestimate, as many cases go unreported. Now imagine the harm caused globally by prescription mistakes.
My aunt was prescribed NSAIDs. She wasn’t told when to stop taking them, so she continued using them for years. The result? Stomach ulcers.
This is why accurate prescription writing isn’t just about following a format — it’s a cornerstone of patient safety and effective care. Every prescription directly impacts a patient’s health and life.
In today’s blog, I will share the basics of prescription writing, including the dos and don’ts. This is especially useful for healthcare professionals authorized to write prescriptions.
Let’s start !!
What is prescription?

A prescription is a written order from a healthcare provider to a pharmacist, instructing them to prepare and dispense medicine for a patient. It’s a direct communication between the provider and the pharmacist and then a patient
The clearer the prescription, the safer it is for the patient.
3 Essential Components of a Prescription
Prescription writing involves three essential components. Understanding each part can significantly improve patient care:
1 Patient and Prescriber Information
2. Drug Details
3. Authentication
“Going into some details of each component.”
1. Patient and Prescriber’s Information.
This includes comprehensive details about both the healthcare provider and the patient.
Example:
For a patient: Full name, address, age (especially for children under 12), and allergies (if any).And
For a prescriber: Full name, address, and professional registration number.
(A prescriber is any healthcare professional eligible to write a prescription)
Why is patient information so important?
- It ensures the right medication is given to the right person, reducing the risk of harm
- Age matters: Dosages often vary for children and adults. For example, a 5-year-old might require 5 ml of syrup, while an adult might need a 500 mg tablet of the same drug.
- Allergies are critical: Allergies are often ignored on a prescription. Allergic reaction can cause a significant harm to a patient. Healthcare provider must ask about and note allergies on the prescription. This allows pharmacists to avoid medications that could trigger allergic reactions and offer safe alternatives if needed.
2. Drug Details and Instructions (Rx and Sig)
This is the most vital part of any prescription. It must include:
- · Drug name (Use the generic name whenever possible.)
Why ?
Writing the generic name gives patients flexibility to choose a brand that fits their budget and ensures availability across pharmacies. It also reduces bias toward specific brands.
· Clearly mentioned dosage form — Specify whether it’s a tablet, syrup, injection, cream, etc
(example: Tablets / Syrup/ Injection/ Cream/Ointment)
· Strength of Drug
Example : 500mg or 100mg/5ml
· Clear instructions for use (Sig) — Include dosage, frequency, and timing.
Example: 1 tablet PO (by mouth) TID (three times daily) after meals.
· Duration of treatment- Specify when to start and stop the medication, or provide tapering instructions if necessary
Example: 1 tablet PO (by mouth) TID (three times daily) after meals for 7 days
“An accurate and complete prescription minimizes risks and maximizes benefits. Incomplete prescriptions, on the other hand, can lead to confusion and harm, as patients often lack the medical knowledge to interpret them correctly”
3. Authentication of a Prescriber
Healthcare providers must include their full name, designation, and medical registration number on the prescription.
A “signature and stamp” of a prescriber in manual prescription is essential to be closed to the final medication listed. Leaving blank spaces can be dangerous, as someone could add unauthorized medications. Always ensure there’s no extra space after the final entry.
Why is authentication important?
It makes the prescription trustworthy and prevents tampering.
Common Mistakes in Prescription Writing (and How to Avoid them)
Prescription errors are a serious issue, costing lives and money. In the UK alone, errors in primary care are associated with over 700 deaths annually and cost £98.5million.
Let’s look at the most common mistakes and how to prevent them.
Mistake 1: Using Confusing abbreviations
Abbreviations can be misunderstood, leading to errors.
For example:
· “U” or “u” for units — can be mistaken as zero or four.
A full form of “units” Should be written.
· “QD” (once daily) can be confused with “QID” (four times daily).
So write in bracket (Daily) with QD and (four times daily) with QID
· “µg” for microgram — frequently misread as “mg”
So write “microgram” in full form
. “ IU” can be confused with IV or 10.
So IU should be written in full form as “International Unit”
- “D/C” can mean “discharge” or “discontinue.” Use the full form to avoid confusion.
Mistake 2: Dosage and Unit Mistakes
Over 50% of prescribing errors are related to dosage. Be especially cautious with decimal points:
- Avoid trailing zeros (e.g., write “1” instead of “1.0” to prevent it from being misread as “10”).
- Always use leading zeros (e.g., write “0.5” instead of “.5” to prevent it from being misread as “5”).
Mistake 3: Incorrect Quantity Notation
- Quantities ≥1 gram should be written in grams (e.g., “2 g”).
- Quantities <1 gram but ≥1 milligram should be written in milligrams (e.g., write “500 mg” instead of “0.5 g”).
- Quantities <1 milligram should be written in micrograms (e.g., write “100 micrograms” instead of “0.1 mg”).
Mistake 4: illegible handwriting
In Manual Prescription Poor Handwriting can cause serious errors. Illegible prescriptions can lead to serious medication errors, potentially causing harm or even fatalities.
Studies have shown 58.5% of handwritten prescriptions had illegible handwriting,
To avoid this:
- Write clearly or print prescriptions.
- Where possible, use digital prescriptions.
Manual Prescription vs. Digital Prescription
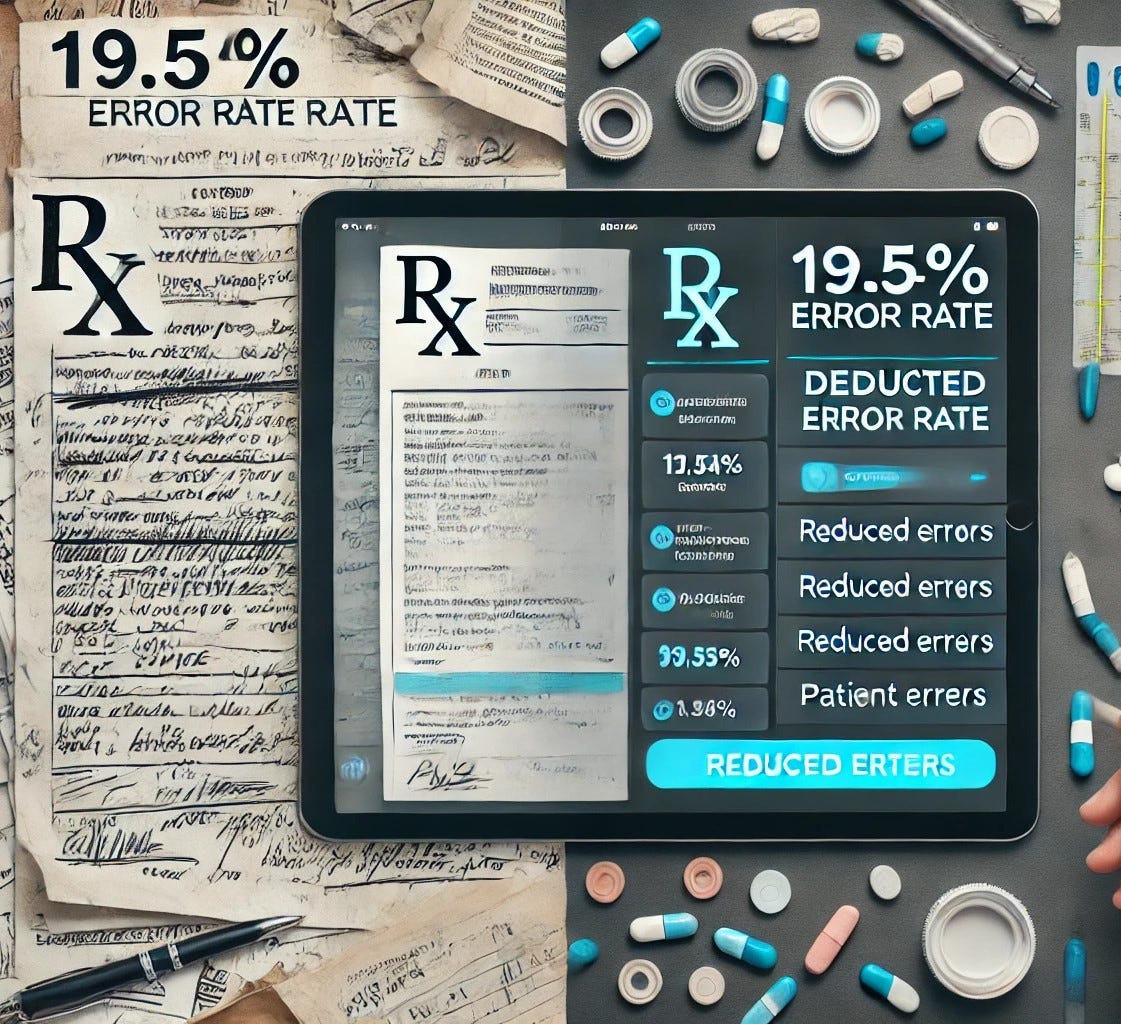
. Manual prescriptions are handwritten and more prone to errors. Studies show error rates of around 19.54%.
. Digital prescriptions (e-prescriptions) are generated electronically, reducing errors and improving clarity. Whenever possible, opt for digital methods to enhance patient safety.
A General Tip for Healthcare Providers
Healthcare providers should make it a visit nearby pharmacies occasionally. Observing their workflows and discussing practical challenges with pharmacists can offer valuable insights. Ask pharmacists for feedback on common issues they face with prescriptions and suggestions for improvement. This is particularly important for primary care or family physicians and any healthcare provider working in an outpatient setting
A brief Prescription Format: Key Elements
Header
The top section of a prescription should include:
- Complete prescriber information (name, address, contact details).
- Complete patient information (full name, address, and date of birth).
Body
The central part of the prescription includes:
- Drug name and strength (in capital letters for clarity).
- Quantity to be dispensed (in both words and figures for controlled substances).
- Clear dosage instructions.
- Duration of treatment.
- Refill information.
Footer
The footer should include:
- Prescriber’s signature and stamp.
- The date of issuance, close to the signature for authenticity.
Conclusion
Proper prescription writing is a critical skill that directly impacts patient safety and healthcare outcomes. Each prescription is more than just a set of written instructions — it’s a vital communication tool between healthcare providers, pharmacists, and patients.
By following clear documentation protocols, avoiding dangerous abbreviations, and maintaining attention to detail, we can prevent thousands of medication errors. Whether using paper or electronic prescriptions, the principles remain the same:
- Clear communication
- Accurate documentation
- Unwavering dedication to patient safety
Mastery of prescription writing comes from practice and a commitment to precision. Small details matter immensely because patient lives depend on them. Upholding high standards in our daily practice ensures that every prescription serves its intended purpose safely and effectively.
Do you have additional tips or experiences about prescription writing that could help other healthcare professionals avoid patient harm?
Share your thoughts in the comments — every voice matters. Thank you!



Very well written Dr hasaam.
I just want to share one personal experience,one doctor wrote 6 u on a discharge slip for regular insulin for a diabetic patient.
His family read it as 60 and was giving it TID so imagine a patient getting 180 unit of insulin instead of 18 units .so she went into hypoglycemic coma and ultimately developed severe hypoglycemic brain injury.
So such a mistake can be devastating for patient .
Thanks for this reminder
Thank you, Dr. Nighat, for sharing your experience.
I’m so sorry to hear about the patient’s situation—it’s heartbreaking to see how a single mistake can have such a devastating impact. This really highlights the importance of vigilance in our work. Studies show that one of the most common and significant errors in healthcare is medication errors.
To address this, we have made patient safety a priority in our Healthcare Quality and Patient Safety course. We have included dedicated sessions that specifically focus on medication errors to help healthcare professionals minimize risks and prevent harm.
Thank you once again for sharing your story. It’s a powerful reminder for all of us to be extra careful and cautious, especially when it comes to writing prescriptions, to protect the patients who trust us.